Turning the Tide Violence Intervention Program (TTVIP)
On This Page
Your support can save a life!
Visit Giving and scroll down in the drop-down menu to select "MUSC Violence Prevention Program."
Violence is one of the leading causes of death and injury for youth and young adults in the US and disproportionally impacts vulnerable and minority populations. Physicians know that people who experience violence often need more than medical care to promote recovery and break cycles of violence.
The MUSC Health Turning the Tide Violence Intervention Program (TTVIP) violence intervention patient advocates provide care and wrap around services to violently injured patients treated at MUSC Health. This program is based on a public health model that recognizes the complex interpersonal, social, economic, and environmental root causes of violence. It is a trauma-informed, patient-centered program designed to include healthcare and community resources to improve intervention and support services for victims of violence.
What are our services?
The MUSC Health TTVIP offers assessment, support, wrap around services, referrals, and long-term follow-up to individuals at risk of violence, and victims of violent injuries and their families. The program provides a comprehensive model of care that intersects the nature of trauma, social determinants of health, and violence.
How does it work?
Our trained care team members engage with at-risk and injured patients at their bedside; assesses patients risk factors and goals; establishes a plan that promotes physical, social, and mental health recovery; and connects the patients and their families with MUSC & community resources that may strengthen support networks, improve social, education, and employment outcomes and prevent repeat violence. We focus on patients between the ages of 12 to 30 that are at risk or experience interpersonal and community violence, but we provide support and services to other patients in need of assistance.
We partner with other community groups and law enforcement to promote violence deterrence and intervention strategies to support neighborhoods experiencing high rates of community violence.
Who are our partners?
We partner with both MUSC Health resources and local community agencies. Within MUSC, we network with the MUSC Advocacy Program (MAP), Trauma and Resiliency and Recovery Program (TRRP), MUSC National Crime Victims Center (NCVC), MUSC Level 1 Adult and Pediatric Trauma Center, and other providers that provide care to patients that experience violence and trauma.
Within the community, we partner with a variety of community, governmental, non-profit agencies, and victim service groups including:
- Criminal justice victim advocates
- School systems and education programs
- Employment programs
- Arts and recreations programs
- Food and housing non-profits
- Family counseling services
- Mental health and substance abuse programs
- Local law enforcement agencies
What are the areas we serve?
We provide care and support to all patients in need of our services. The primary areas served in the Lowcountry include Charleston, Beaufort, Colleton, Dorchester, and Berkley counties.
What is our expertise and research?
Members of the team have vast experience in the field of violence including nationally published violence prevention research, advocacy, education, non-profit work, injury prevention, and community violence intervention. See Research and Related News for some of our publications and work.
Our program is supported by The Health Alliance for Violence Interventions (HAVI) organization. The HAVI builds and connects a network of hospital-based intervention programs and promotes equity for victims of violence.
Violence Prevention & Intervention Research
The TTVIP team and their colleagues are involved in research to advance our understanding of violence-related injuries and how we can prevent them and support survivors.
Grant: Bridging the Gaps: Individual and Community-Level Risk Factors for Non-Lethal Firearm Injuries in the United States
Funder: National Collaborative on Gun Violence Research (NCVGR)
Principle Investigators: Dr. Avery Nathans (University of Toronto), Dr. Deb Kuhls (UNLV School of Medicine), Dr. Ashley Hink (Medical University of South Carolina), Dr. Fred Rivara (University of Washington)
Grant: Lowcountry Rising Above Violence - Healthcare and Community Violence Prevention & Intervention Program
Funder: Department of Justice, Office of Juvenile Justice and Delinquency Prevention
Program Leads: Ashley Hink, MD, MPH; Christa Green, MPH (Medical University of South Carolina)
Grant: Pediatric Firearm Deaths: A Mixed-Methods Analysis of Individual- and Situation-Level Factors Contributing to Racial and Ethnic Disparities (R03)
Funder: National Institute of Child Health and Human Development
Principal Investigator: Amy Hunter, MPH, PhD (UConn Health)
Research Support: Christa Green, MPH (Medical University of South Carolina)
Andrews A, Oddo E, Killings X, Gastineau K, Hink A.
Pediatric Firearm Injury Mortality Update. Pediatrics. 2022. Accepted, pending publication.
Bonne S, Hink A, Violano P, Allee L, Duncan T, Burke P, Fein J, Kozyckyj T, Shapiro D, Bakes K, Kuhls D, Bulger E, Dicker R.
Understanding the makeup of a growing field: A committee on trauma survey of the national network of hospital-based violence intervention programs.
Ruggiero KJ, Anton MT, Davidson TM, deRoon-Cassini TA, Hink AB.
It is time to prioritize complete trauma care
Gastineau KAB, Stegall CL, Lowrey LK, Giourgas BK, Andrews AL
Improving the Frequency and Documentation of Gun Safety Counseling in a Resident Primary Care Clinic
Hink AB.
Using State Hospitalization Databases to Improve Firearm Injury Data-A Step in the Right Direction
Oddo ER, Maldonado L, Hink AB, Simpson AN, Andrews AL.
Increase in Mental Health Diagnoses Among Youth With Nonfatal Firearm Injuries
Hink AB, Atkins DL, Rowhani-Rahbar A.
Not All Survivors Are the Same: Qualitative Assessment of Prior Violence, Risks, Recovery and Perceptions of Firearms and Violence Among Victims of Firearm Injury
Doucette ML, Green C, Necci Dineen J, Shapiro D, Raissian KM.
Impact of ShotSpotter Technology on Firearm Homicides and Arrests Among Large Metropolitan Counties: a Longitudinal Analysis, 1999-2016
Silver AH, Andrews AL, Azzarone G, Bhansali P, Hjelmseth E, Hogan AH, O'Connor KM, Romo N, Parikh K.
Engagement and Leadership in Firearm-Related Violence Prevention: The Role of the Pediatric Hospitalist
Gastineau KAB, Andrews AL.
Pediatric Hospitalists at the Front Line of Gun Violence Prevention: Every Patient Encounter Is an Opportunity to Promote Safe Gun Storage.
Hink AB, Bonne S, Levy M, Kuhls DA, Allee L, Burke PA, Sakran JV, Bulger EM, Stewart RM.
Firearm injury research and epidemiology: A review of the data, their limitations, and how trauma centers can improve firearm injury research
DiVietro S, Beebe R, Grasso D, Green C, Joseph D, Lapidus GD
A dual-method approach to identifying intimate partner violence within a Level 1 trauma center
Kuhls DA, Campbell BT, Burke PA, Allee L, Hink A, et al.
American College of Surgeons Committee on Trauma. Survey of American College of Surgeons Committee on trauma members on firearm injury: Consensus and opportunities.
Dicker RA, Gaines BA, Bonne S, Duncan T, Violano P, Aboutanos M, Allee L, Burke PA, Maskiakos PT, Hink A, Kuhls DA, Shapiro D, Stewart RM.
Violence intervention programs: A primer for developing a comprehensive program for trauma centers.
Hink AB, Toschlog E, Waibel B, Bard M.
Risks go beyond the violence: Association between intimate partner violence, mental illness, and substance abuse among females admitted to a rural Level I trauma center
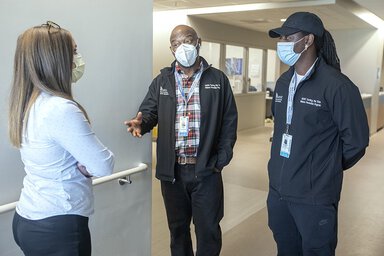
Meet The Team
Ashley Hink, M.D., MPH
Medical Director
Associate Professor of Acute Care Surgery
Christa Green, MPH
Program Director
Kristen Moldenhauer, MA
Early Intervention Advocate
Chantelle Mitchell
Violence Intervention Advocate
Adrianna Bellamy, BSPH
Adult Trauma Injury Prevention Coordinator
Cat Yetman, BS
Violence Intervention Advocate
Herbert Jenkins, D. Min
Violence Intervention Advocate
Claire Jacoby, BA
Research Assistant
Clinical Champions
Chris Streck, M.D.
MUSC Department of Surgery, Division of Pediatric Surgery
Morsal Tahouni, M.D.
MUSC Department of Emergency Medicine
Elizabeth Oddo, M.D.
MUSC Pediatric Liaison